Add adults with type 2 diabetes, HbA1c ≥ 9% despite metformin, BMI ≥ 30 kg/m², and not yet on advanced metabolic agents to the metabolic-intervention study candidate list.
|
Identify trial candidates
Add metastatic colorectal cancer patients treated this year, whose tumors are MSI-high or dMMR and who have ECOG 0–1, to the immunotherapy trial candidate roster.
|
Identify trial candidates
Page infection-prevention nurses to evaluate inpatients who have Foley catheters placed more than 48 hours ago and a urine culture of at least 100,000 CFU/mL for CAUTI.
|
Prevent hospital infections
Add lung-cancer patients with an EGFR mutation confirmed on molecular testing, a creatinine clearance above 30 mL/min, and no prior targeted therapy to the candidate list for EGFR-targeted clinical trials.
|
Identify trial candidates
Add metastatic breast-cancer patients seen this year who are HER2-low, have ECOG 0–1, and have not received antibody-drug therapy to the Phase III candidate list for new HER2-low trials.
|
Identify trial candidates
Generate the hip-fracture form and alert the orthopedic data abstractor for hip-fracture admissions discharged this week that meet national registry criteria but lack a registry entry.
|
Automate registry mapping
Pre-fill the stroke quality-registry form and notify the stroke program for patients with discharge summaries finalized in the past 24 hours that include an NIHSS score and lack an entry in the stroke quality registry.
|
Automate registry mapping
Auto-enroll all adults with confirmed pathogenic BRCA1 or BRCA2 variants who are not yet enrolled in the hereditary-cancer registry and send them yearly MRI reminders.
|
Automate registry mapping
Auto-fill the NAACCR record and alert the registrar for new malignant pathology reports from the last 24 hours with tumor site or histology not yet present in the registry.
|
Automate registry mapping
Alert nursing leadership to perform and log oral care for ventilated ICU patients intubated for more than 48 hours who have no oral-care documentation in the last 12 hours.
|
Prevent hospital infections
Prompt the care team to draw blood cultures and consider line replacement for patients with central lines in place for 7 days or more, a fever above 100.4 °F, and no blood culture drawn in the past 24 hours.
|
Prevent hospital infections
Send stewardship alerts to stop prophylactic antibiotics or document a rationale for all postoperative patients from yesterday who are still receiving prophylactic antibiotics more than 24 hours after incision closure.
|
Prevent hospital infections
Invite immunocompromised adults aged 19–64 without documentation of the PCV-20 vaccine to a nurse-run vaccine clinic via MyChart.
|
Boost preventive screening
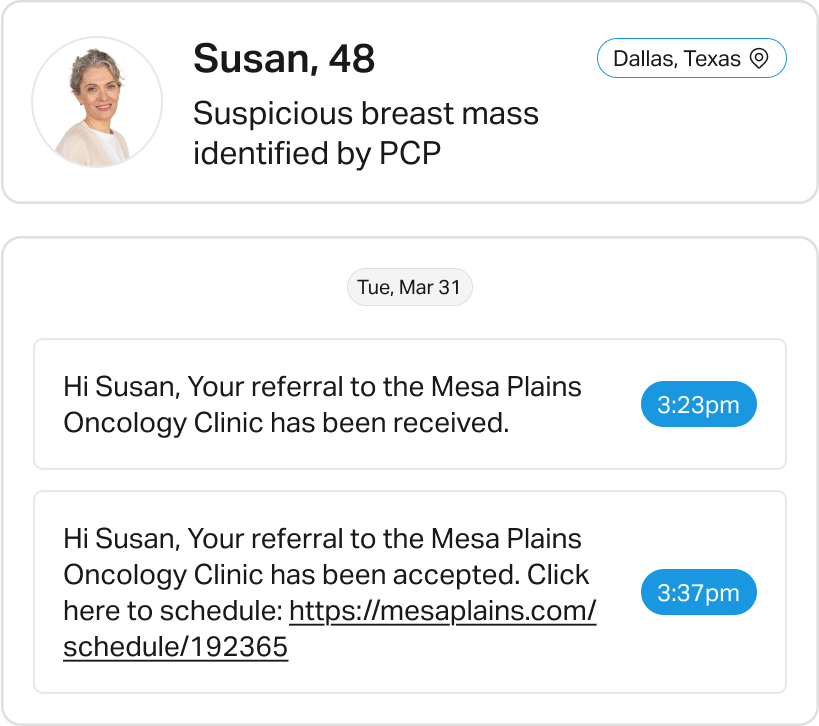
Auto-refer patients with a BRCA mutation or first-degree family history of early breast cancer who have never completed genetics counseling or high-risk screening to genetics services and prompt them to schedule an MRI.
|
Boost preventive screening
Add a mammography order suggestion to the pre-chart note for women aged 40–74 with an upcoming primary-care visit and no mammogram documented in the past 2 years.
|
Boost preventive screening
Send an SMS with a self-scheduling link for stool testing or colonoscopy to adults aged 45–75 who visited primary care this year and lack up-to-date colorectal-cancer screening.
|
Boost preventive screening
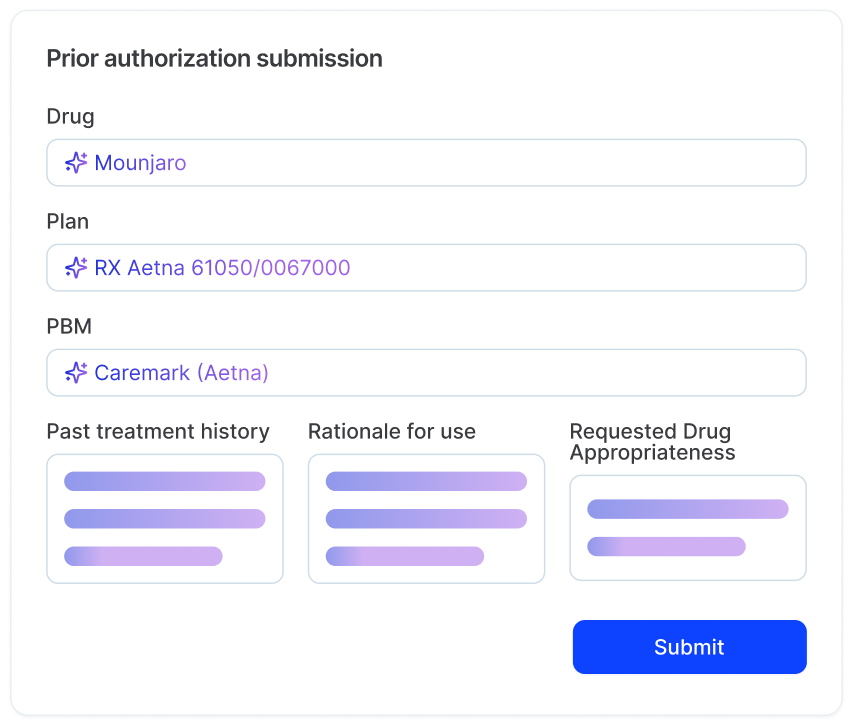
Request an authorization extension for scheduled cardiac catheterization cases with authorizations expiring before the procedure date, and reschedule the case if the payer denies the extension.
|
Streamline prior authorization
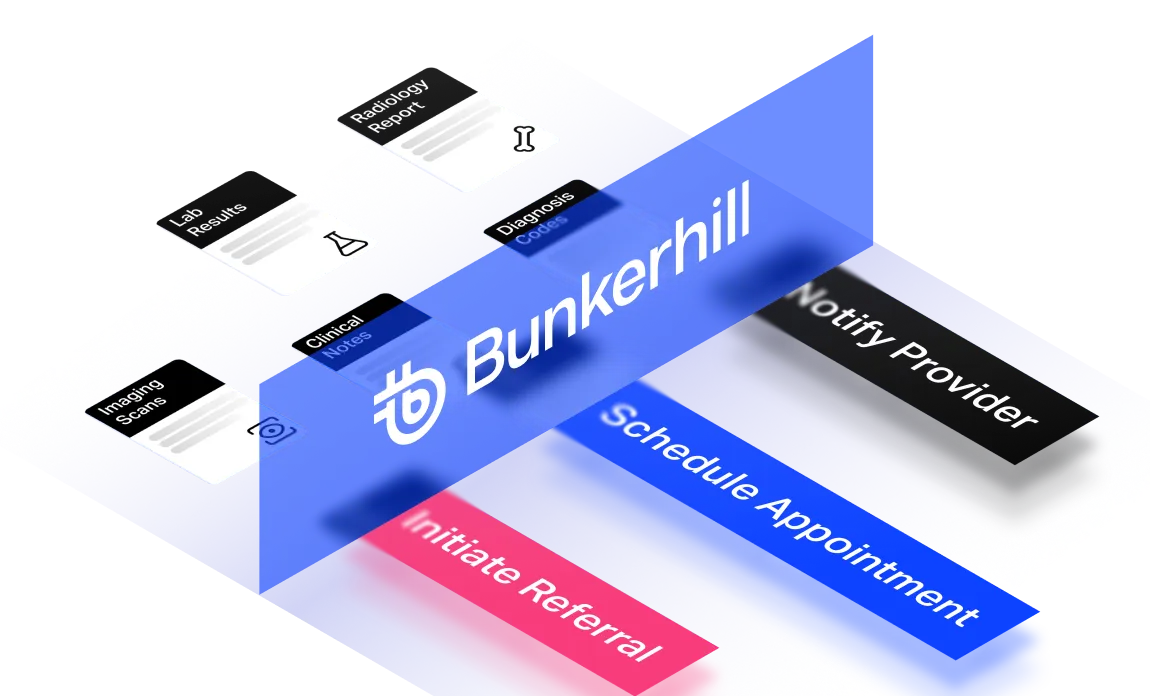
Attach required conservative-therapy documentation to outpatient knee MRI orders for sports-injury patients scheduled within 5 days who lack this documentation, file the authorization with the payer, and update radiology upon approval.
|
Streamline prior authorization
Auto-add a tobacco-use code and update the RAF value for all Medicare Advantage COPD stays this quarter that lack a documented tobacco-use code affecting RAF scoring.
|
Improve case-mix accuracy
Auto-submit prior authorization, notify the team, and initiate appeal if denied for any order placed in the last 24 hours flagged as requiring prior authorization, still lacking an auth code after 12 hours, and with service needed within 7 days.
|
Streamline prior authorization
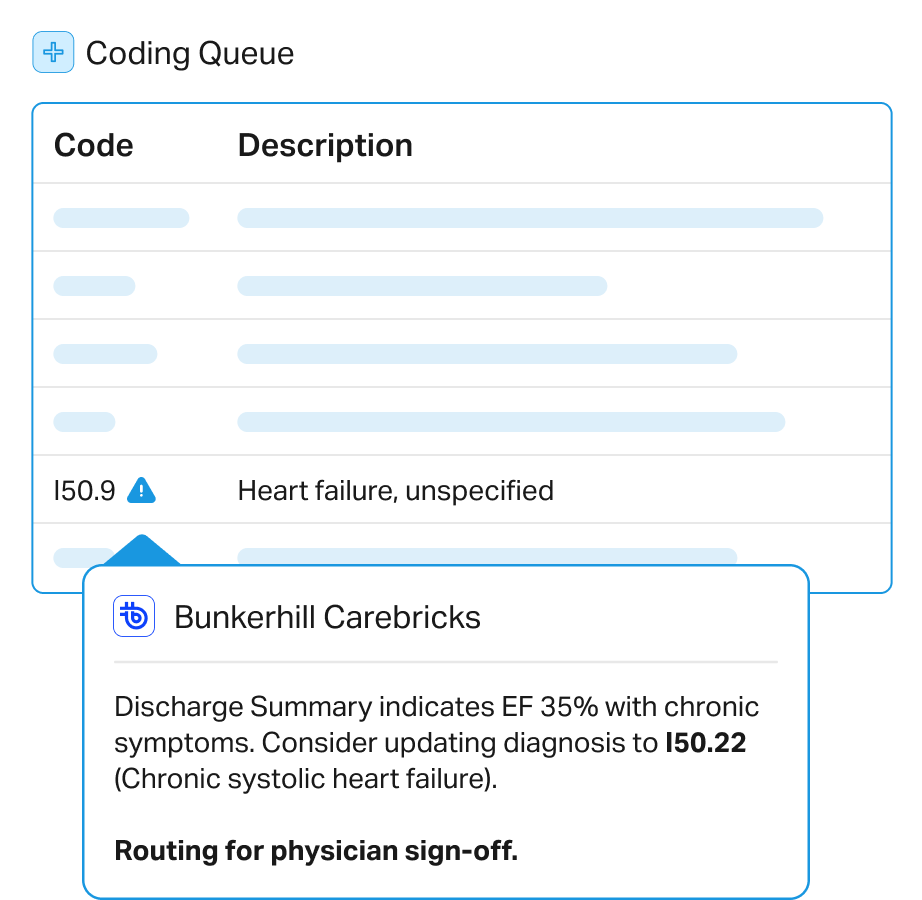
Draft corrected ICD-10 and DRG updates for revenue integrity for inpatient echocardiograms finalized this week with LVEF ≤ 40% that are billed under unspecified heart-failure codes.
|
Improve case-mix accuracy
Compile the authorization packet for newly diagnosed metastatic lung-cancer patients prescribed osimertinib who lack payer authorization 24 hours before the planned start date, submit the packet to the payer, and alert the pharmacy upon approval.
|
Streamline prior authorization
Prompt the physician to add an addendum documenting AKI stage for recent discharges with sepsis and acute kidney injury noted in progress notes, where the summary omits creatinine trends that meet KDIGO stage 2.
|
Improve case-mix accuracy
Send a coding query with a ready-to-sign update to the attending physician for each COPD admission this quarter whose notes mention chronic respiratory failure but lack the ICD-10 code J96.10.
|
Improve case-mix accuracy
Queue an echocardiogram order and text the valve clinic about same-day slots for patients who received routine chest CTs in the last 90 days, where Bunkerhill’s FDA-cleared algorithm detects severe aortic-valve calcium and no echocardiogram is currently ordered.
|
Address actionable findings
Notify the electrophysiology referral queue with patient details for those whose echocardiogram reports from the past 6 months show LVEF ≤ 40% and who lack a systolic heart-failure ICD code.
|
Address actionable findings
Send an alert to the incidental-nodule clinic work queue for patients with a chest CT report from the last week that mentions a solid nodule ≥ 8 mm and who have no pulmonology note or follow-up imaging order.
|
Address actionable findings
Message the PCP with statin guidance and a cardiology referral link for each patient who had a routine chest CT in the past month with moderate or severe coronary calcium detected by Bunkerhill’s FDA-cleared algorithm.
|
Address actionable findings